Concept explainers
Adapting to Host Defenses Surface proteins called HLAs allow white blood cells to detect HIV particles and fight an infection. In a recent study, scientists tested whether HIV is adapting to this host defense. They did so by looking at the frequency of a specific mutation (1135X) in HIV. This “escape mutation” helps the virus avoid detection by a version of the HLA protein (HLA-B*51) that is common in some regions of the world, but not in others. FIGURE 20.19 shows the percentage of HIV-positive people who had HIV with the 1135X mutation. Data were collected at medical centers from several parts of the world.
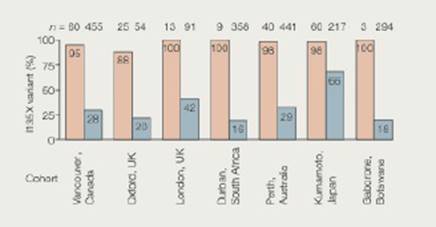
FIGURE 20.19 Regional variation in the frequency of the 1135X escape mutation among HIV-positive people. For each region, pink bars represent the percentage of people whose blood cells have HLA-B*51. and thus cannot detect 1135X mutants. Blue bars represent the percentage of people with other versions of the HLA protein. These people have blood cells that can detect and fight HIV even if it has the 1135X mutation.
1. What percentage of people with H LA-B*51 in Vancouver had HIV with the escape mutation for this protein?
Want to see the full answer?
Check out a sample textbook solution
Chapter 20 Solutions
Biology: The Unity and Diversity of Life (MindTap Course List)
- 1. Match each vocabulary term to its best descriptor A. affinity B. efficacy C. inert D. mimic E. how drugs move through body F. how drugs bind Kd Bmax Agonist Antagonist Pharmacokinetics Pharmacodynamicsarrow_forward50 mg dose of a drug is given orally to a patient. The bioavailability of the drug is 0.2. What is the volume of distribution of the drug if the plasma concentration is 1 mg/L? Be sure to provide units.arrow_forwardDetermine Kd and Bmax from the following Scatchard plot. Make sure to include units.arrow_forward
- Choose a catecholamine neurotransmitter and describe/draw the components of the synapse important for its signaling including synthesis, packaging into vesicles, receptors, transporters/degradative enzymes. Describe 2 drugs that can act on this system.arrow_forwardThe following figure is from Caterina et al. The capsaicin receptor: a heat activated ion channel in the pain pathway. Nature, 1997. Black boxes indicate capsaicin, white circles indicate resinferatoxin. a) Which has a higher potency? b) Which is has a higher efficacy? c) What is the approximate Kd of capsaicin in uM? (you can round to the nearest power of 10)arrow_forwardWhat is the rate-limiting-step for serotonin synthesis?arrow_forward
 Human Physiology: From Cells to Systems (MindTap ...BiologyISBN:9781285866932Author:Lauralee SherwoodPublisher:Cengage Learning
Human Physiology: From Cells to Systems (MindTap ...BiologyISBN:9781285866932Author:Lauralee SherwoodPublisher:Cengage Learning Biology: The Unity and Diversity of Life (MindTap...BiologyISBN:9781305073951Author:Cecie Starr, Ralph Taggart, Christine Evers, Lisa StarrPublisher:Cengage Learning
Biology: The Unity and Diversity of Life (MindTap...BiologyISBN:9781305073951Author:Cecie Starr, Ralph Taggart, Christine Evers, Lisa StarrPublisher:Cengage Learning Human Heredity: Principles and Issues (MindTap Co...BiologyISBN:9781305251052Author:Michael CummingsPublisher:Cengage Learning
Human Heredity: Principles and Issues (MindTap Co...BiologyISBN:9781305251052Author:Michael CummingsPublisher:Cengage Learning- Essentials of Pharmacology for Health ProfessionsNursingISBN:9781305441620Author:WOODROWPublisher:Cengage





